Hip Replacement

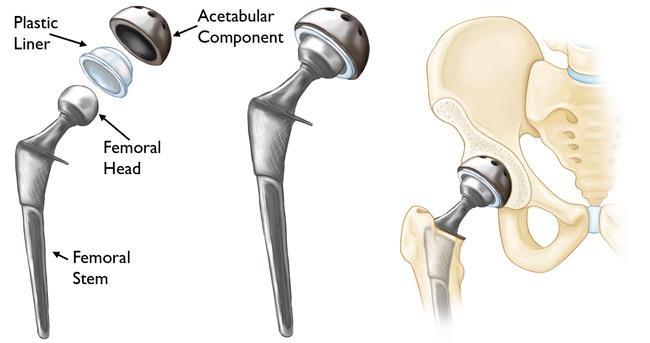
In a total hip replacement (also called total hip arthroplasty), the damaged bone and cartilage is removed and replaced with prosthetic components. The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur. The femoral stem may be either cemented or “press fit” into the bone. A metal or ceramic ball is placed on the upper part of the stem. This ball replaces the damaged femoral head that was removed. The damaged cartilage surface of the socket(acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place. A plastic, ceramic, or metal spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.
Robotic hip replacement Advantages of robotic surgery
More accurate placement and alignment of hip implants based on the surgical plan.
- Less likelihood of hip dislocation.
- Reduced blood loss.
- Replication of the feeling of a natural hip.
- Preservation of healthy bone.
Step 1: Personalized surgical plan

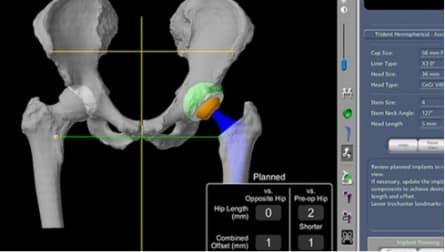
Prior to surgery, a CT scan of your hip joint is taken in order to generate a 3D virtual model of your unique anatomy. The 3D model helps your doctor see things he or she can’t typically see with an x-ray alone. This additional information helps your doctor determine the optimal size, placement and positioning of your implant.
Step-2: Range-of-motion assessment
Throughout your procedure, Mako provides real-time data to your surgeon. This allows them to continuously assess the movement and tension of your new joint, and adjust your surgical plan if desired.
Step-3: Arthritic bone removal
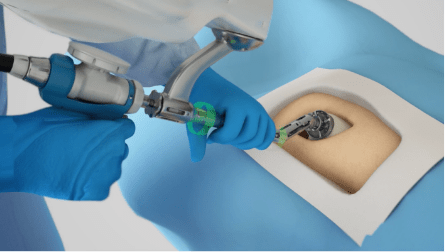
In the operating room, your surgeon guides Mako’s robotic arm to remove the arthritic bone and cartilage from the hip. A virtual boundary provides tactile resistance to help the surgeon stay within the boundaries defined in your surgical plan.
Implant placement
As the surgeon prepares to place the implant into its final position, the robotic-arm guides the implant at the desired angle defined in the surgical plan. This helps ensure the placement and alignment of the implant are performed according to plan.
Causes of Hip Pain
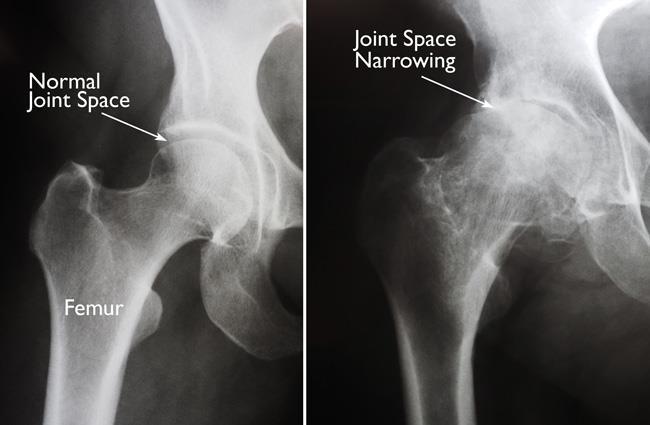
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
Osteoarthritis: This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older and often in individuals with a family history of arthritis. The cartilage cushioning the bones of the hip wears away. The bones then rub against each other, causing hip pain and stiffness. Osteoarthritis may also be caused or accelerated by subtle irregularities in how the hip developed in childhood. Rheumatoid arthritis: This is an autoimmune disease in which the synovial membrane becomes inflamed and thickened. This chronic inflammation can damage the cartilage, leading to pain and stiffness. Rheumatoid arthritis is the most common type of a group of disorders termed “inflammatory arthritis.” Post-traumatic arthritis: This can follow a serious hip injury or fracture. The cartilage may become damaged and lead to hip pain and stiffness over time. Osteonecrosis: An injury to the hip, such as a dislocation or fracture, may limit the blood supply to the femoral head. This is called osteonecrosis (also sometimes referred to as “avascular necrosis”). The lack of blood may cause the surface of the bone to collapse, and arthritis will result. Some diseases can also cause osteonecrosis. Childhood hip disease: Some infants and children have hip problems. Even though the problems are successfully treated during childhood, they may still cause arthritis later on in life. This happens because the hip may not grow normally, and the joint surfaces are affected.
Recommended for
There are several reasons why your doctor may recommend hip replacement surgery. People who benefit from hip replacement surgery often have:
- Hip pain that limits everyday activities, such as walking or bending
- Hip pain that continues while resting, either day or night
- Stiffness in a hip that limits the ability to move or lift the leg
- Inadequate pain relief from anti-inflammatory drugs, physical therapy, or walking supports
Candidates for Surgery
There are no absolute age or weight restrictions for total hip replacements.
Recommendations for surgery are based on a patient’s pain and disability, not age. Most patients who undergo total hip replacement are age 50 to 80, but orthopaedic surgeons evaluate patients individually. Total hip replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis. Preparations An evaluation with an orthopaedic surgeon consists of several components. Medical history: Your orthopaedic surgeon will gather information about your general health and ask questions about the extent of your hip pain and how it affects your ability to perform everyday activities. Physical examination: This will assess hip mobility, strength, and alignment. X-rays: These images help to determine the extent of damage or deformity in your hip. Other tests: Occasionally other tests, such as a magnetic resonance imaging (MRI) scan, may be needed to determine the condition of the bone and soft tissues of your hip.
Recovery
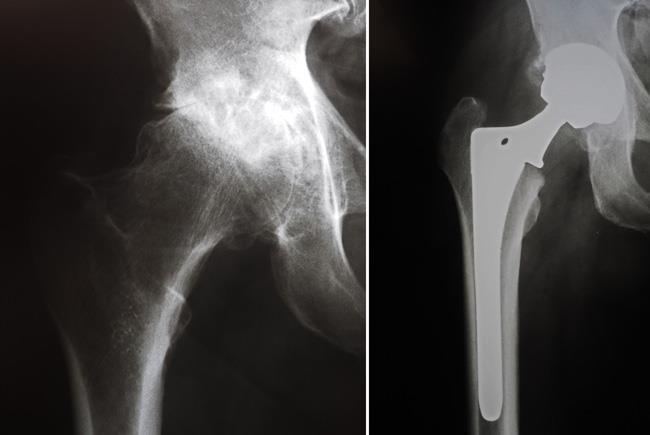
The surgical procedure usually takes from 1 to 2 hours. Your orthopaedic surgeon will remove the damaged cartilage and bone and then position new metal, plastic, or ceramic implants to restore the alignment and function of your hip. X-rays before and after total hip replacement. In this case, non-cemented components were used. After surgery, you will be moved to the recovery room where you will remain for several hours while your recovery from anesthesia is monitored. After you wake up, you will be taken to your hospital room or discharged to home.
The success of your surgery will depend in large measure on how well you follow your orthopaedic surgeon’s instructions regarding home care during the first few weeks after surgery.
Wound Care
You may have stitches or staples running along your wound or a suture beneath your skin. The stitches or staples will be removed approximately 2 weeks after surgery. Avoid getting the wound wet until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.
Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength. Be sure to drink plenty of fluids.
Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within 3 to 6 weeks following surgery. Some discomfort with activity and at night is common for several weeks. Your activity program should include:
- A graduated walking program to slowly increase your mobility, initially in your home and later outside
- Resuming other normal household activities, such as sitting, standing, and climbing stairs
- Specific exercises several times a day to restore