Shoulder Replacement
Symptoms
Severe shoulder pain that interferes with everyday activities, such as reaching into a cabinet, dressing, toileting, and washing.
- Moderate to severe pain while resting. This pain may be severe enough to prevent a good night’s sleep.
- Loss of motion and/or weakness in the shoulder.
- Failure to substantially improve with other treatments such as anti-inflammatory medications, cortisone injections, and/or physical therapy.
Causes
Several conditions can cause shoulder pain and disability, and lead patients to consider shoulder joint replacement surgery.
Osteoarthritis (Degenerative Joint Disease)
Osteoarthritis is an age-related wear-and-tear type of arthritis. It usually occurs in people 50 years of age and older, but may occur in younger people, too. The cartilage that cushions the bones of the shoulder softens and wears away. The bones then rub against one another. Over time, the shoulder joint slowly becomes stiff and painful.
Unfortunately, there is no way to prevent the development of osteoarthritis. It is a common reason people have shoulder replacement surgery.
Rheumatoid Arthritis
This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed inflammatory arthritis.
Post-traumatic Arthritis
This can follow a serious shoulder injury. Fractures of the bones that make up the shoulder or tears of the shoulder tendons or ligaments may damage the articular cartilage over time. This causes shoulder pain and limits shoulder function.
Rotator Cuff Tear Arthropathy

Avascular Necrosis (Osteonecrosis)
Avascular necrosis, or osteonecrosis, is a painful condition that occurs when the blood supply to the bone is disrupted. Because bone cells die without a blood supply, osteonecrosis can ultimately cause destruction of the shoulder joint and lead to arthritis. Chronic steroid use, deep sea diving, severe fracture of the shoulder, sickle cell disease, and heavy alcohol use are all risk factors for avascular necrosis.
Severe Fractures
A severe fracture of the shoulder is another common reason people have shoulder replacements. When the head of the upper arm bone is shattered, it may be very difficult for a doctor to put the pieces of bone back in place. In addition, the blood supply to the bone pieces can be interrupted. In this case, a surgeon may recommend a shoulder replacement. Older patients with osteoporosis are most at risk for severe shoulder fractures.
Failed Previous Shoulder Replacement Surgery
Although uncommon, some shoulder replacements fail, most often because of implant loosening, wear, infection, and dislocation. When this occurs, a second joint replacement surgery — called a revision surgery — may be necessary.
Types
Shoulder replacement surgery is highly technical. It should be performed by a surgical team with experience in this procedure. There are different types of shoulder replacements. Your surgeon will evaluate your situation carefully before making any decisions. They will discuss with you which type of replacement will best meet your health needs. Do not hesitate to ask which type of implant will be used in your situation, and why that choice is right for you.
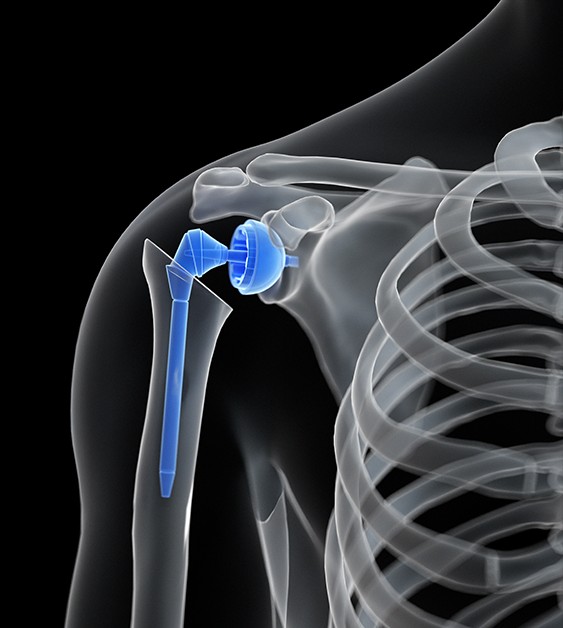
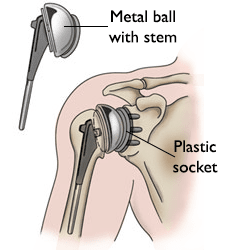
Total Shoulder Replacement
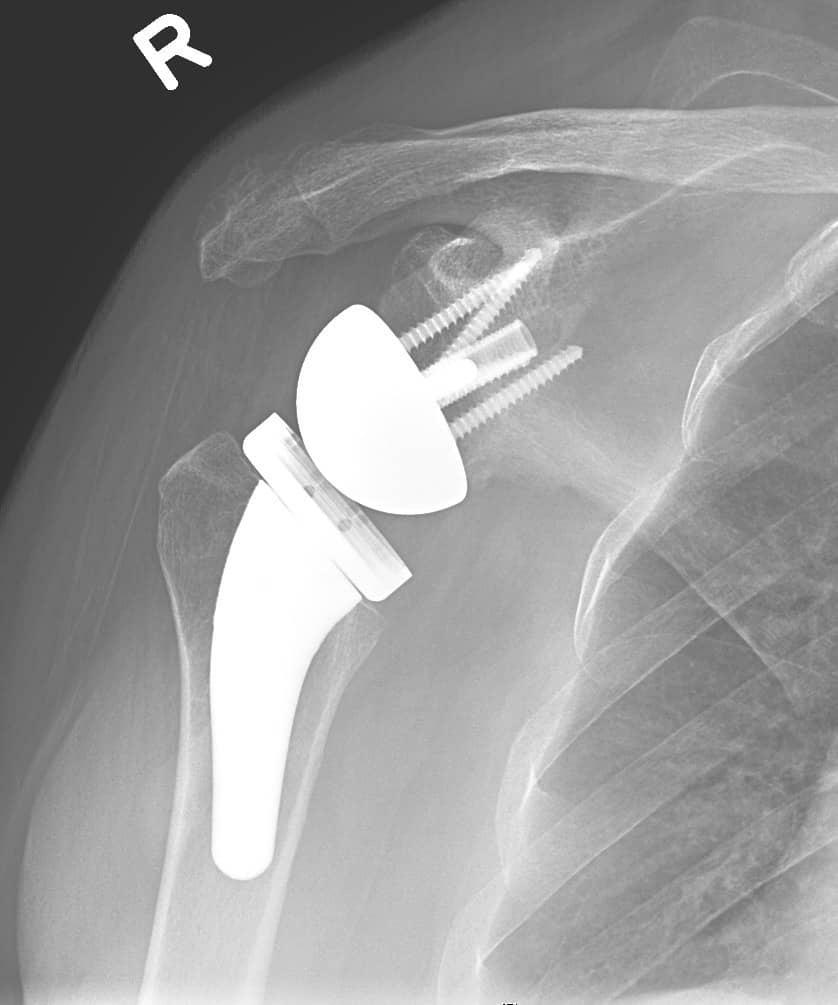
The standard total shoulder replacement involves replacing the arthritic joint surfaces with a highly polished metal ball attached to a stem, and a plastic socket.
These components come in various sizes. They may be either cemented or press fit into the bone. If the bone is of good quality, your surgeon may choose to use a non-cemented (press-fit) humeral component. If the bone is soft, the humeral component may be implanted with bone cement. In most cases, an all-plastic glenoid (socket) component is implanted with bone cement.
- Implantation of a glenoid component is not advised if:
- The glenoid has good cartilage
- The glenoid bone is severely deficient
- The rotator cuff tendons are irreparably torn
Resurfacing Hemiarthroplasty
Resurfacing hemiarthroplasty involves replacing just the joint surface of the humeral head with a cap-like prosthesis without a stem. With its bone-preserving advantage, it offers those with arthritis of the shoulder an alternative to the standard stemmed shoulder replacement. Resurfacing hemiarthroplasty may be an option for you if:
- The glenoid still has an intact cartilage surface
- There has been no fresh fracture of the humeral neck or head
- There is a desire to preserve humeral bone
Reverse Total Shoulder Replacement
Another type of shoulder replacement is called reverse total shoulder replacement. Reverse total shoulder replacement is used for people who have:
- Completely torn rotator cuffs with severe arm weakness
- The effects of severe arthritis and rotator cuff tearing (cuff tear arthropathy)
- Had a previous shoulder replacement that failed
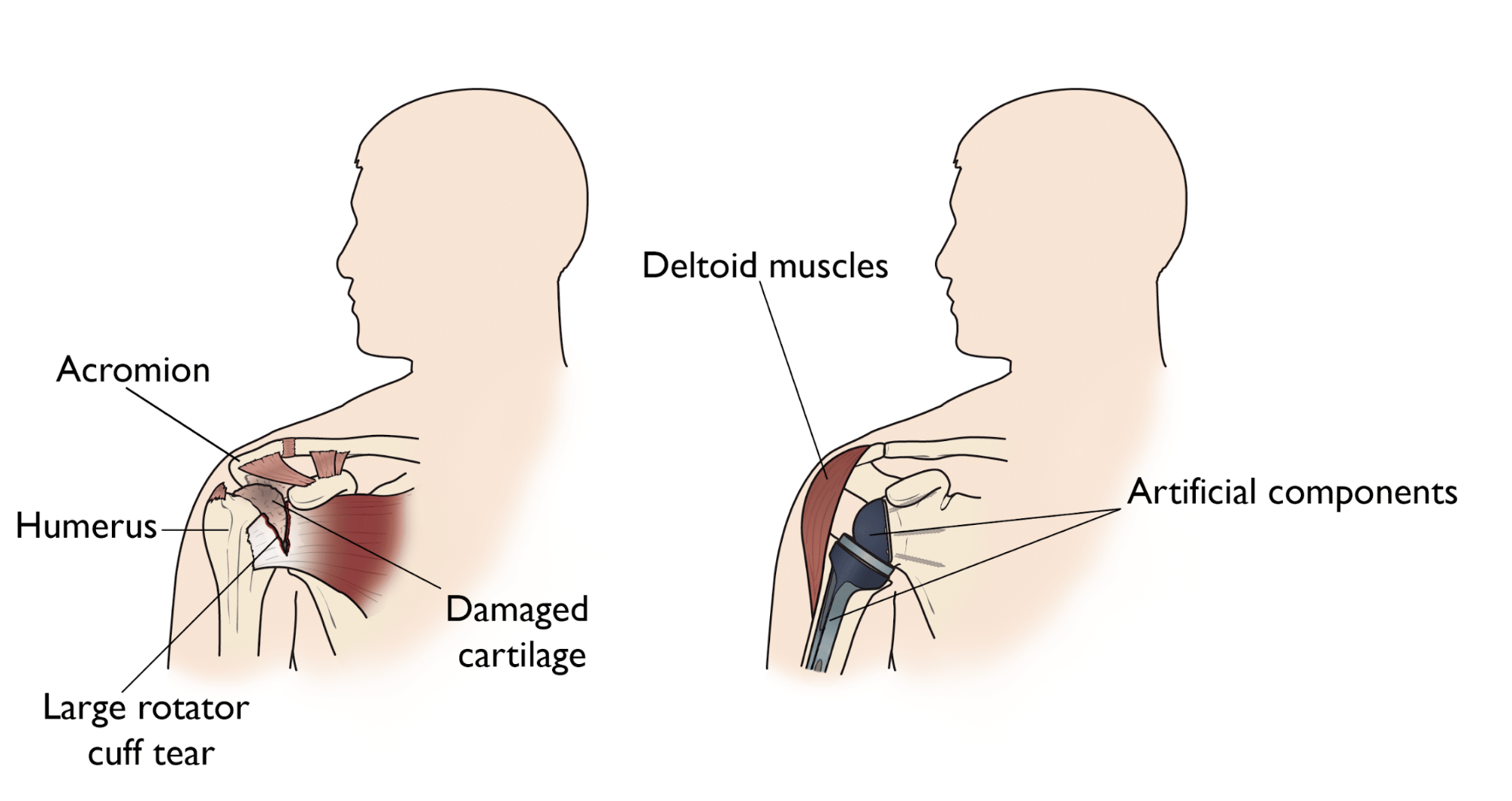
(Left) Rotator cuff arthropathy. (Right) The reverse total shoulder replacement allows other muscles — such as the deltoid — to do the work of the damaged rotator cuff tendons.
Recommended for
The decision to have shoulder replacement surgery should be a cooperative one between you, your family, your family physician, and your orthopaedic surgeon. There are several reasons why your doctor may recommend shoulder replacement surgery. People who benefit from surgery often have:
- Severe shoulder pain that interferes with everyday activities, such as reaching into a cabinet, dressing, toileting, and washing.
- Moderate to severe pain while resting. This pain may be severe enough to prevent a good night’s sleep.
- Loss of motion and/or weakness in the shoulder.
- Failure to substantially improve with other treatments such as anti-inflammatory medications, cortisone injections, and/or physical therapy.
- A medical history. Your orthopaedic surgeon will gather information about your general health and ask you about the extent of your shoulder pain and your ability to function.
- A physical examination. This will assess shoulder motion, stability, and strength.
- X-rays. X-rays help to determine the extent of damage in your shoulder. They can show loss of the normal joint space between bones, flattening or irregularity in the shape of the bone, bone spurs, and loose pieces of cartilage or bone that may be floating inside the joint.
- Other tests. Occasionally, your doctor may order blood tests, a computed tomography (CT) scan, a magnetic resonance imaging (MRI) scan, or a bone scan to determine the condition of the bone and soft tissues of your shoulder.

Recovery
The procedure to replace your shoulder joint with an artificial device usually takes about 2 hours. After surgery, you will be moved to the recovery room, where you will remain for several hours while your recovery from anesthesia is monitored. After you wake up, you will be taken to your hospital room.
Your medical team will give you several doses of antibiotics to prevent infection. Most patients are able to eat solid food and get out of bed the day after surgery. You will most likely be able to go home on the first, second, or third day after surgery.
Rehabilitation
A careful, well-planned rehabilitation program is critical to the success of a shoulder replacement. You usually start gentle physical therapy soon after the operation. Your surgeon or physical therapist will provide you with a home exercise program to strengthen your shoulder and improve flexibility.
Your Recovery At Home
When you leave the hospital, your arm will be in a sling. You will need the sling to support and protect your shoulder for the first 2 to 6 weeks after surgery, depending on the complexity of your surgery and your surgeon’s preference. Wearing a sling will protect your shoulder after surgery.
Wound care: You will have staples running along your wound or a suture beneath your skin. The staples will be removed several weeks after surgery. A dissolving suture beneath your skin will not require removal. Avoid soaking the wound in water until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing.
Activity: Exercise is a critical component of home care, particularly during the first few weeks after surgery. Follow your surgeon’s home exercise plan to help you regain strength. Most patients are able to perform simple activities such as eating, dressing, and grooming, within 2 weeks after surgery. Some pain with activity and at night is common for several weeks after surgery. You are not allowed to drive a car for 2 to 6 weeks after surgery.