Total Knee Replacement
Knee Replacement Procedure
There are four basic steps to a knee replacement procedure:
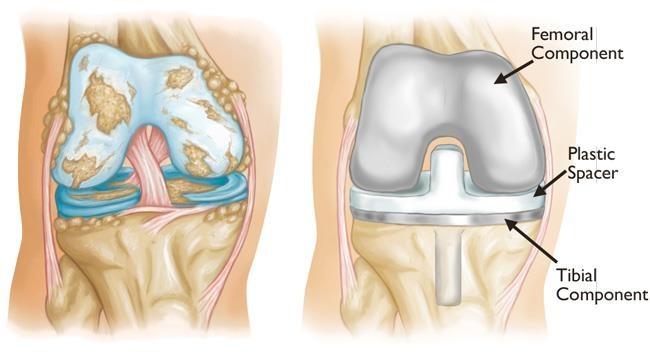
Prepare the bone: The damaged cartilage surfaces at the ends of the femur and tibia are removed along with a small amount of underlying bone.
Position the metal implants: The removed cartilage and bone is replaced with metal components that recreate the surface of the joint. These metal parts may be cemented or “press-fit” into the bone.
Resurface the patella: The undersurface of the patella (kneecap) is cut and resurfaced with a plastic button. Some surgeons do not resurface the patella, depending upon the case.
Insert a spacer: A medical-grade plastic spacer is inserted between the metal components to create a smooth gliding surface.
Symptoms
There are several reasons why your doctor may recommend knee replacement surgery. People who benefit from total knee replacement often have:
- Severe knee pain or stiffness that limits everyday activities, including walking, climbing stairs, and getting in and out of chairs. It may be hard to walk more than a few blocks without significant pain and it may be necessary to use a cane or walker
- Moderate or severe knee pain while resting, either day or night
- Chronic knee inflammation and swelling that does not improve with rest or medications
- Knee deformity — a bowing in or out of the knee
- Failure to substantially improve with other treatments such as anti-inflammatory medications, cortisone injections, lubricating injections, physical therapy, or other surgeries
Causes
The most common cause of chronic knee pain and disability is arthritis. Although there are many types of arthritis, most knee pain is caused by just three types: osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.
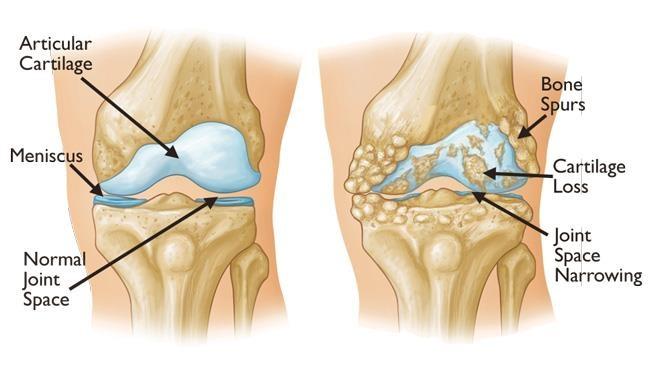
Rheumatoid arthritis: This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed “inflammatory arthritis.”
Post-traumatic arthritis: This can follow a serious knee injury. Fractures of the bones surrounding the knee or tears of the knee ligaments may damage the articular cartilage over time, causing knee pain and limiting knee function.
Types
Recommended for
There are no absolute age or weight restrictions for total knee replacement surgery.
Recommendations for surgery are based on a patient’s pain and disability, not age. Most patients who undergo total knee replacement are age 50 to 80, but orthopaedic surgeons evaluate patients individually. Total knee replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
Preparations
An evaluation with an orthopaedic surgeon consists of several components:
Medical history: Your orthopaedic surgeon will gather information about your general health and ask you about the extent of your knee pain and your ability to function.
Physical examination: This will assess knee motion, stability, strength, and overall leg alignment.
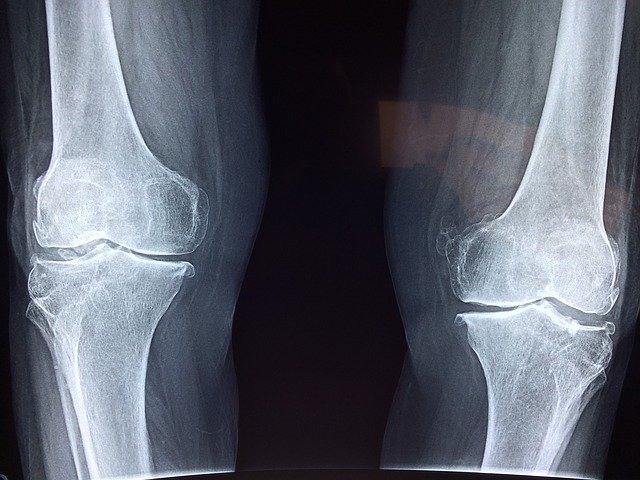
X-rays: These images help to determine the extent of damage and deformity in your knee.
Other tests: Occasionally blood tests or advanced imaging, such as a magnetic resonance imaging (MRI) scan, may be needed to determine the condition of the bone and soft tissues of your knee.Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether total knee replacement is the best method to relieve your pain and improve your function. Other treatment options — including medications, injections, physical therapy, or other types of surgery — will also be considered and discussed. In addition, your orthopaedic surgeon will explain the potential risks and complications of total knee replacement, including those related to the surgery itself and those that can occur over time after your surgery.
Recovery
The surgical procedure usually takes from 1 to 2 hours. Your orthopaedic surgeon will remove the damaged cartilage and bone, and then position the new metal and plastic implants to restore the alignment and function of your knee.After surgery, you will be moved to the recovery room, where you will remain for several hours while your recovery from anesthesia is monitored. After you wake up, you will be taken to your hospital room or discharged to home.
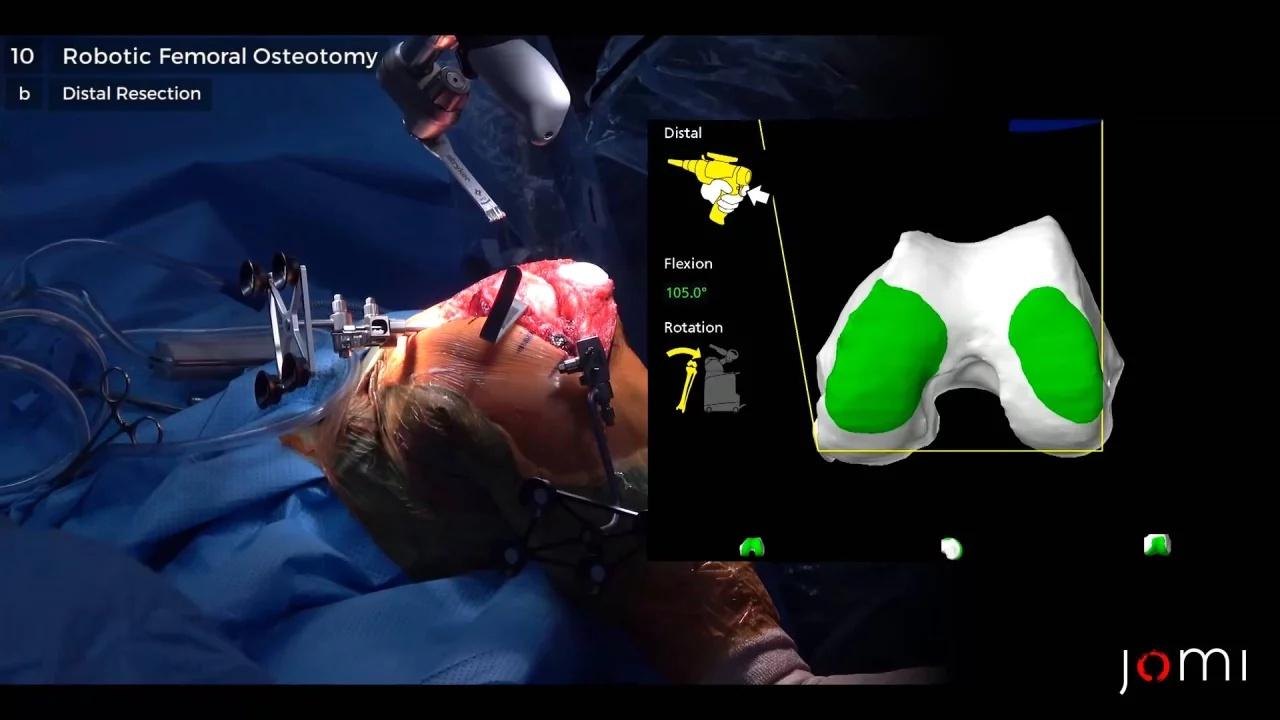
Robotic assisted replacements
The term “robotic surgery” refers to the use of programmable devices to perform a wide variety of surgical tasks. These are not intended to replace the surgeon but rather to provide assistance.Robots present a tool in which surgeons can do surgical procedures while minimizing human error and maximizing operative accuracy.

Robotic TKR was developed to improve bone preparation accuracy and decrease the possibility of outliers to guarantee a longer prosthesis lifespan. Adequate restoration of the mechanical axis in TKA is associated with a decrease in polyethylene wear and a lower revision arthroplasty rate.
Robotic system stops the saw when bone resection begins to go outside predetermined parameters set in the preoperative plan. It improves the surgeon’s ability to perform the knee alignment and protect the soft tissue components like the MCL, PCL, and the popliteal artery. It creates a three-dimensional model of the patient’s knee from CT images to exactly calculate bone resection, prosthesis size, and position.
Robotic TKA is characterized by decreased postoperative pain and requirement of analgesia, better HB levels, quicker restoration of the straight leg raise test, a short stay in the hospital, and better knee flexion on discharge in comparison with a conventional replacement technique.